CASE STUDIES
BOARD CERTIFIED NEUROSURGEON
FELLOWSHIP TRAINED IN MINIMALLY INVASIVE & COMPLEX SPINE SURGERY
Case Studies
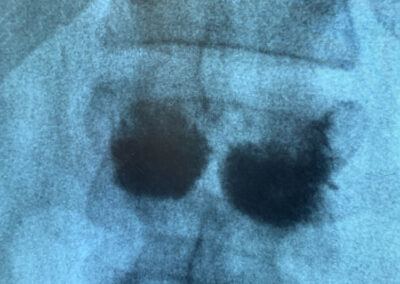
Brain Cases
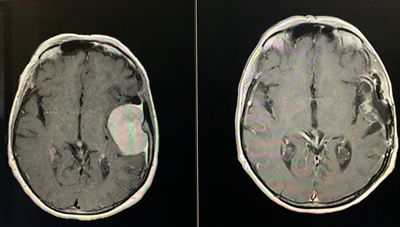
Case 1
Elderly patient had tripped and fallen down, hitting his head on the floor. A small tumor was found on CT and MRI. Many such tumors do not need surgery or intervention. We followed it with MRI every year. It showed no growth at 3 years.
Other such tumors can grow in size; at that time other options such as radiosurgery or surgical resection are discussed
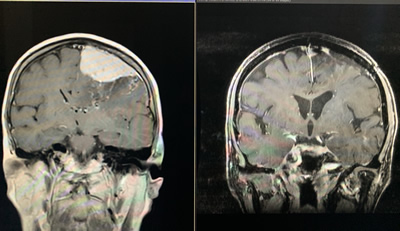
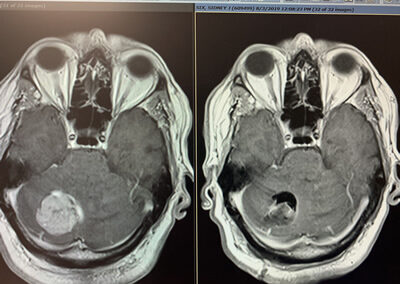
Case 2
76 yr old patient admitted through ER because of right sided weakness, with difficulty using right hand and walking. Large tumor was found on MRI, next to many critical structures. Chemotherapy is typically not an option for the kind of tumor that was suspected; it was too large for radiation therapy. Surgery was the best option to remove the pressure from the brain. Tumor was completely resected without complications. There was immediate improvement in right sided weakness after surgery. Patient was discharged home 3 days after surgery. When seen in clinic at 3 months, strength was now normal.
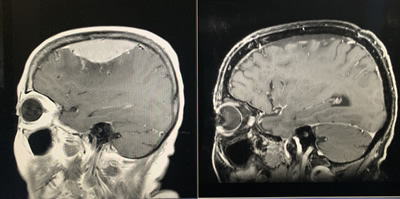
Case 3
A 62-year-old patient admitted to the ER with speech difficulty and seizures. Large tumor found on MRI. Chemotherapy is typically not an option for the type of tumor that was suspected, and it was too large for radiation therapy. Surgery was the best option to remove the pressure from the brain. The tumor was completely resected without any complications. Her speech difficulty improved significantly over the next few days and over the course of the next several months was normal.
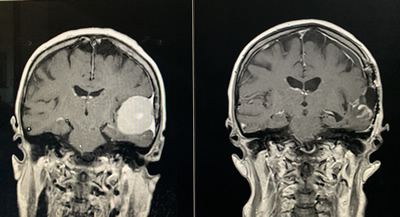
Case 4
A 74-year-old patient admitted through the ER with a several week history of headache and worsening difficulty with walking and balance problems. A tumor was found on the patient’s brain MRI. Given the location of the tumor, surgical resection was the best option, with chemotherapy and radiation if needed. The tumor was completely resected without complications. The patient had an immediate improvement in balance and headaches. When seen in clinic 3 weeks later, headaches had completely resolved and balance was back to normal.
Cervical Spine (Neck)
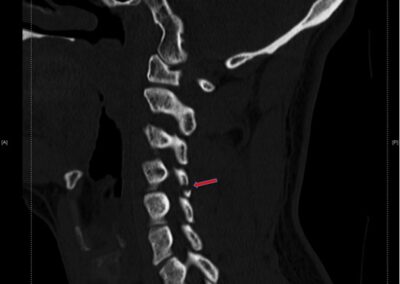
Case 1
A 24-year-old suffered a fracture of one of the joints in the neck. Given the nature of the fracture, surgery vs cervical collar were discussed. The patient was placed in a cervical collar and followed regularly/closely/every few weeks in clinic. After several months of observation in collar and repeat X-rays, we were able to remove the collar and allow the patient to return to work, avoiding surgery.
Case 2
A 65-year-old surgeon had a complaint of severe left-sided neck pain and numbness going into his arm. It did not improve with nonsurgical treatments including medications, therapy, massage, and injections. MRI showed severe left-sided nerve impingement. It was treated with a cervical foraminotomy via a less than 1-inch incision. This also allowed preservation of motion at that level. The patient had immediate resolution of his symptoms. He was able to return to work 2 days later.
https://www.spine-health.com/video/cervical-posterior-foraminotomy-video
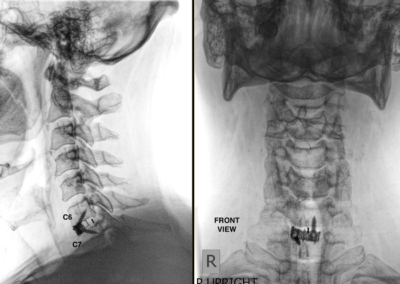
Case 3
A 56-year-old patient had a complaint of severe right-sided arm pain, numbness, and weakness along with some right leg numbness as well. Symptoms had worsened rapidly despite treatment with multiple different types of medications. MRI showed a large disc herniation compressing the right side of the spinal cord. While many such patients can be treated without surgery, in this case, because of the severe symptoms surgery was performed (C6-7 ACDF). He had immediate relief of his symptoms, his strength was already almost back to normal when he woke up from surgery. He was discharged home the same day.
https://www.spine-health.com/treatment/spinal-fusion/acdf-anterior-cervical-discectomy-and-fusion
Case 4
A 66-year-old had complained of difficulty using both her arms and legs, with weakness of her right arm and right leg. MRI showed spinal cord compression at C4-5. C4-5 ACDF was performed. These symptoms improved significantly after surgery.
Case 5
A 59-year-old patient presented with a long history of neck pain, with worsening severe arm pain, with profound weakness to arms and legs and difficulty walking. Imaging showed severe degenerative changes with spinal cord and nerve compression, which was expected given how long the symptoms had been present. Surgery was done just from the front of the neck. There were no complications. Removing the pressure from the spinal cord stopped the progression of her weakness, and preserved the ability to use arms and be able to walk. The patient had some residual pain and numbness, which was expected given how long the symptoms have been present. Before performing surgeries for treatment of severe neurological symptoms and findings on MRI such as this, I have very extensive discussions with the patients about risks, benefits, and expectations.
Case 6
A 75-year-old patient presented with neck pain, arm pain, severe arm and leg weakness, and inability to walk. Imaging showed very severe degenerative changes with spinal cord and nerve compression. Very extensive discussions were held with the patient and her family. The patient underwent a combined surgery from the front and back of the neck to remove the pressure from the nerves and spinal cord. The patient did very well with significant improvement in arm and leg strength. In fact, arm and leg strength was almost back to normal. The patient was able to walk with drastically improved balance and stability.
Thoracic and Lumbar Spine
Case 1
A physician in his late 30s had presented with a several year history of low back pain and left leg sciatica. Symptoms had worsened despite extensive nonsurgical treatments including medications, therapy, massage and injections. MRI showed left-sided nerve impingement at two levels. This was treated with a lumbar laminectomy / microdiscectomy via a less than 1-inch incision. This also allowed preservation of motion at both levels. The patient had immediate resolution of his symptoms. He was able to return to work in a few days.
Case 2
A student in her early 20s had presented with acute onset severe upper lumbar spine pain after falling down a hill while hiking on vacation. CT showed an L1 fracture. Different treatment options were discussed. Initially the plan was to treat it with pain medications and bracing, allowing it to heal over the next few months. However, given her inability to take time off from school for recovery, she would have missed a year of education. We then discussed and performed a kyphoplasty procedure through less than 5mm incisions. She had immediate improvement in pain. She was able to walk without narcotic pain medications after waking from surgery, and was discharged less than 24 hours after it was performed.
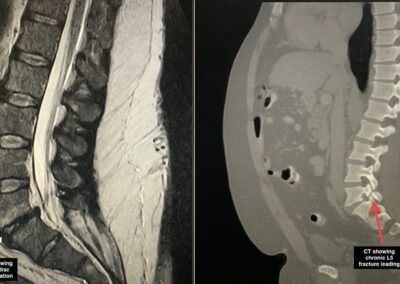
Case 3
A patient in his mid 50s had presented with many years of low back pain and sciatica, which had worsened significantly over the last 1 year. His CT, MRI, and xrays showed chronic stress fracture (referred to as a pars defect or fracture) leading to the conditions of spondylolisthesis, stenosis, and instability of the spine when standing up. He had failed non-surgical treatments and given the nature of his condition, surgery was recommended. He had L5-S1 fusion using a minimally invasive technique. He reported significant improvement in his severe back and leg pain postoperatively.
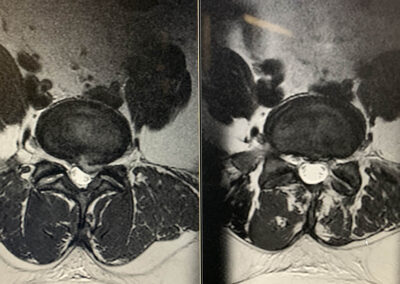
Case 4
A patient in her 50s presented with progressively worsening balance and gait difficulty. Her MRI showed a large spinal cord tumor in the upper part of her thoracic spine causing severe spinal cord compression. If left untreated, a tumor such as this can grow and cause neurologic deficits such as paralysis. There were no viable non-surgical treatment options, therefore surgery was performed. The tumor was completely removed; which fortunately was benign. She had significant improvement in her balance.
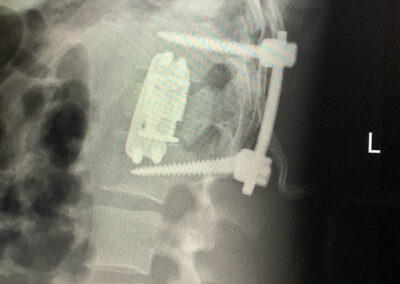
Case 5
A patient his early 20s presented with numbness, weakness, loss of bowel and bladder function after a motor vehicle accident. He had suffered a L1 burst fracture causing a spinal cord injury. He underwent a combination of mini-open and open surgery to remove pressure from the spinal cord and stabilize the spine with hardware. Given that he was in his early 20s, another goal was to fuse the fewest number of levels possible to allow motion at other levels. He reported immediate improvement in numbness and strength. He was able to walk without assistance in a few weeks, and over the next few months he regained control of his bowel and bladder function as well.
Case 6
A patient in his late 30s presented with severe low back pain and sciatica. His MRI and CT showed a complex sacral fracture which was not amenable to non-surgical treatment. A mini-open surgical technique along with computerized image guided technology was used to place hardware and stabilize his fractures. He had profound improvement in his pain and was able to stand up and walk the next day.